Why Choose Dental Wellness of Lexington?
Whether you’re seeking preventive care, looking for an emergency dentist near you, want to perfect your smile with veneers, or anything in between, our accomplished dentists in Lexington specialize in improving smiles for the long-term.

Personalized
Dental Care
Every treatment plan is comprehensively customized for the patient’s needs, preferences, and goals.

State-of-the-Art
Dental Care
Our modern facility features private treatment rooms and the latest technological advances in the dental field.

Same-Day
Dental Emergencies
Knocked-out tooth? Serious mouth pain? Dental Wellness of Lexington can welcome you in without delay.

Comprehensive
Dentistry Options
We want to be your trusted oral healthcare home for all dental needs, from simple checkups to specialty treatment.

Teaching Center
for Dentists
You're in great hands. Dentists from all around the U.S. learn about implants and sedation from Dr. Feck.

Meet Dr. Patel, the newest member of our team of excellent dentists
MEET DR. PATELOur Patients Say It Best
Central Kentucky Center
for Implant Dentistry
Replacements
The prolonged loss of natural teeth can make it difficult to chew favorite foods and even speak with confidence while also actively harming your health. Here in Lexington, our top-rated dentists would like to help you explore the transformative power of dental implants, which are virtually indistinguishable from natural teeth in look, form, and function! From a single dental implant to implant dentures, our experienced dentists can perform every stage of treatment – including the surgical components – right here in our state-of-the-art facility with the latest technological advancements for optimal convenience and quality.
Learn More About Dental Implants
Central Kentucky Center
for Sedation Dentistry
Dental Anxiety
Dental phobia is a serious problem that affects patients of all ages, often leading to skipped appointments and worsening oral health problems. Thankfully, IV sedation can create a calm and pleasant environment that soothes even the most frazzled nerves in the treatment chair! At Dental Wellness of Lexington, our doctors have trained with some of the world’s most prominent sedation dental specialists, and they currently teach sedation courses on a nationwide basis too, proving that their expertise in this advanced service can be relied on wholeheartedly by patients in need.
Learn More About IV Sedation
Comprehensive Dental Treatments


I Need A Checkup
& Cleaning


I Have A Broken or
Chipped Tooth


I Am Missing One
or More Teeth


I Am Afraid/ Nervous
of the Dentist


I Want A Straighter
Smile


I Am in Pain or
Had an Accident


I Am Worried About
Bleeding Gums


I Want To Improve
My Smile
Dental Insurance & Financing Expert
Paying for important dental care shouldn’t have to be stressful or overcomplicated. Jacqueline can help you navigate the variety of options available, understand the cost of dentistry, and select the best path forward for your personal budget.
?Ask Jacqueline A Question Explore Your Financial Options
Jacqueline
•Financial Coordinator
Dental Insurance
Looking for a Delta Dental Premier or Cigna dentist near you? We are in-network with a few major PPO dental insurances. Our team can also file claims on your behalf!
In-House Savings Plan
No dental insurance? Don’t worry. Our in-house savings plan offers valuable discounts and free preventive care for a low yearly rate.
Carecredit™ Financing
Payment plans through CareCredit come with little to NO interest and can be used to better manage the cost of big treatment plans.

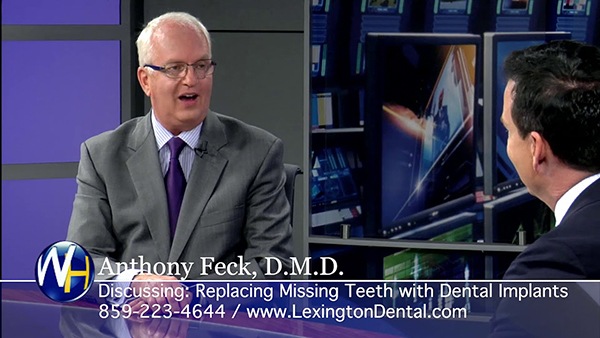
Want to Upgrade
Your Dentures?
Watch our Wellness Hour segment about Dental Implants.
You Asked, We Answered!
Our team at Dental Wellness of Lexington believes strongly in you being an active part of your treatment, which is why we’re always here to provide recommendations, share advice, and answer questions. While you’re more than welcome to talk to our team over the phone or at your next appointment, many patients also like completing some research online beforehand. If that’s the case for you, then read on for the answers to FAQs!
How can I find a female dentist?
Look no further than our Lexington dental office! We’re proud to have three dedicated, talented, and exceptional female dentists, Dr. Maxie Combs, Dr. Carol Wilson, and Dr. Amita Patel. Although their educational backgrounds and journeys to Dental Wellness of Lexington are unique, they share the same passion for delivering world-class dentistry, and they would love to help you achieve your smile goals!
Of course, if you aren’t in the Lexington area, then it may be helpful to ask family, friends, and coworkers for their recommendations. You can also search Google for “female dentist near me,” which can provide you with a list of providers in your area.
What do you do if you can't afford a dentist?
There is a common misconception that dentistry is expensive. In reality, a study from The Journal of Dental Medicine found that every dollar invested in preventive care can save you between $8 and $50 on restorative and cosmetic dentistry. So, the best way to keep your dental treatments affordable is by prioritizing good oral hygiene best practices, like coming in for a checkup and cleaning every six months.
Our team is also proud to offer our patients several financial solutions so cost isn’t the only thing standing in your way of getting the preventive, restorative, and even cosmetic dentistry you desire. We welcome dental insurance, happily accept flexible financing through CareCredit, and offer periodic special offers to help you save on popular treatments.
What level of education is required to be a dentist?
As you may know, becoming a dentist requires years of schooling as well as a commitment to continuing education. The journey begins by earning an undergraduate degree (which is usually in a major that’s heavy in math and science). Then, the aspiring dentist needs to be accepted to one of 67 accredited dental schools in the US. Even after earning their Doctor of Dental Medicine (DMD) or Doctor of Dental Sciences (DDS) and becoming a licensed dentist, they need to pursue additional training annually to stay abreast of the latest techniques and technology.
How do I get emergency dental care?
Priority number one is assessing your situation. If you’re experiencing potentially life-threatening symptoms in tandem with your dental injury (i.e., difficulty swallowing, uncontrollable bleeding, trouble breathing), then you need to visit the ER for medical attention. If you aren’t experiencing any potentially life-threatening symptoms, then your first call should be to our Lexington dental office. We do our best to accommodate emergency patients with same-day treatment. That way, we can restore your beautiful, functional, and pain-free smile ASAP.




